On the 29th June 2013, From Pink to Prevention organised a toxic tour in Central London. The tour took in various sites of significance in relation to cancer prevention – or rather the lack of action on cancer prevention by government offices and other bodies.

At each venue speakers addressed various aspects in relation to the total lack of action on the part of governments and the cancer establishment on the issue of the primary prevention of cancer (ie stopping it before it starts). They discussed their work on the issue and posted up Blue Plaques announcing ‘Cancer Prevention does not live here’ at each site to commemorate the visit.
The notion of ‘toxic tours’ originated in the USA with tours held annually in San Francisco and campaigning groups using ‘bucket brigade tours’ to test the air quality around nearby industries which was harming community health. The tours advocate for civil rights and environmental justice. The first ‘toxic tour’ in the UK was organised by Helen Lynn and the Women’s Environmental Network (WEN) and held in London. Subsequent tours were held in Wales organised jointly with WEN Wales and the Campaign for the Protection of Rural Wales, and in Scotland in conjunction with WEN Scotland. This is the second tour of this kind in London which aimed to highlight the environmental and occupational links to cancers in general and breast cancer in particular.
The tour was organised by The Alliance for Cancer Prevention, Tipping Point Film Fund in conjunction with the Organic Pharmacy.
The Programme for the Walk
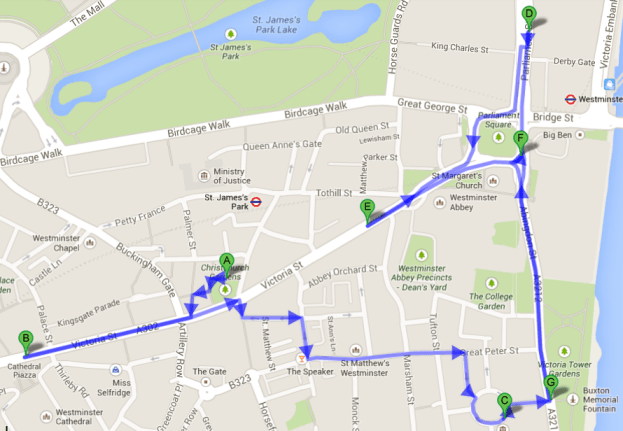
The walk began at the Suffragette statue in Christchurch Gardens, Victoria and en route took in a shopping mall, the Dept. of Health, Dept. of Environment, Food and Rural Affairs, the Dept. for Business, Innovation and Skills and the House of Parliament itself. The tour finished at the Emmeline Pankhurst statue.
 The tour was introduced by Deborah Burton who acknowledging the inspiration from the US and San Francisco tours where activists took members of the general public on alternative walks around polluted districts or installations or visited polluting industries to raise awareness of the health and environmental impact from exposure to contaminated air, soil and water.
The tour was introduced by Deborah Burton who acknowledging the inspiration from the US and San Francisco tours where activists took members of the general public on alternative walks around polluted districts or installations or visited polluting industries to raise awareness of the health and environmental impact from exposure to contaminated air, soil and water.
The London toxic tour route followed a story through daily life represented by a shopping mall, with the wider environment illustrated by a visit to DEFRA; workplace exposure as represented by the Department for Business, Innovation and Skills; and public health, occupational and environmental ill-health outside the Dept. of Health; to the Houses of Parliament where legislation has been non-existent in terms of cancer prevention and finally, to the Emmeline Pankhurst statue, to discuss the political nature of gender, breast cancer and pink washing.
Helen Lynn ~ Our daily life
Maria Arnold ~ Department of Environment, Food and Rural Affairs
Professor Andrew Watterson ~ Department of Health
Professor Andrew Watterson ~ Department for Business, Innovation and Skills
Hilda Palmer ~ UK Parliament
Deborah Burton ~ All Party Parliamentary Group
Dr. Ana Porroche-Escudero ~ Emmeline Pankhurst statue
made by Lin Ho-Chih
photographed by Eve Barker and Helen Lynn
Helen Lynn
Our daily life
Full text is available here (pdf).
The tour’s first stop was at a ‘cathedral’ to the new religion of shopping – the Cardinal Place Shopping Mall. Helen Lynn from the Alliance for Cancer Prevention invited us to come and worship at its altar. Given on average we spend 18 full days shopping a year we do a lot of worshipping!
The question we must ask ourselves is this, what price consumerism? The never ending drive to fuel the greed for cheaper, smaller, faster, lighter and more convenient products purges our planet of resources, and can adversely affect our health right along the production chain from cradle to grave. Many consumers believe – if it’s on sale its safe. But we realise now, nothing could be further from the truth. Less than 10% of chemicals in regular commercial use have been properly tested for health effects.
The WHO conservatively estimates that 24% of human disease and disorders are due, at least in part, to environmental factors which include chemicals exposures (including those at work). [1] At least 28 different cancers have been linked with occupational and environmental exposures. [2] And the International Agency for Research on Cancer (IARC) have identified 449 chemicals and substances which are known, probably or suspected carcinogens many of which are in regular use. [3]
[1] Global assessment of the state-of-the-science of endocrine disruptors- WHO http://www.who.int/ipcs/publications/new_issues/endocrine_disruptors/en/
[2] Environmental and Occupational Causes of Cancer (New Evidence 2005 – 2007) Richard Clapp. Lowell Centre for Sustainable Production. www.sustainableproduction.org
[3] IARC – Agents classified by the IARC Monographs, Volumes 1-102. http://monographs.iarc.fr/ENG/Classification/index.php [Accessed 1/9/2011]
Certain chemicals known as Endocrine Disrupting Chemicals (EDCs) or (hormone disrupting chemicals) interfere with our hormones such as oestrogen or testosterone. Our hormones regulate our endocrine system which is like the bodies messenger system, sending messages to and from cells which control basically everything that is essential to life.
These EDCs may also bio-accumulate in our fat tissue, and the tissues of the animals we eat and be passed down, unwittingly, to future generations crossing the placenta and finding their way into breast milk. 300 synthetic chemicals have been discovered in human body tissues and secretions including breast milk. Although we have known about certain chemicals ability to mimic hormones for a very long time, we have done little to proactively regulate them and there is insufficient testing on chemicals to determine if they are EDCs before they are released onto the market.
There are 800 chemicals which are known or suspected of interfering with our hormones. [4]
Some examples of EDCs are phthalates, which are used to carry fragrances in cosmetics and to soften plastics – they are recognised as the ‘new car’ smell. These chemicals can be found in a variety of consumer products including clothing.
Around 80 billion garments are produced worldwide each year, the equivalent of just over 11 garments a year for every person on the planet. Last year Greenpeace tested 141 items of clothing from brands with shops found here in the cathedral of shopping. They found EDCs and also azo dyes which are used in the dying process of fabrics which can later release cancer causing amines. Phthalates were found in the printed images on textiles. There are hazardous chemicals released throughout the clothing production line, during manufactured, washing, wearing and finally, disposal.
Other examples of EDCs include chemicals like Bisphenol A which was recently taken out of baby feeding bottles but is still widely used to line tin cans and can be found in tooth fillings and in medical devices such as plastic tubing.
Consider the ability of these toxic chemical to accumulate in places no other man-made chemical should be, making their way to the top of the food chain where sits the human child.
Between 137 – 232 toxic chemicals have been found in the umbilical cord blood taken from newborns. 132 of these chemicals are reported to cause cancer in humans/animals, 110 are toxic to the brain or nervous system, and 133 cause developmental and reproductive problems in mammals (humans are also mammals). [5] Other chemicals found in cord blood include Brominated Flame Retardants (BFRs) used to make products flame retardant, Polychlorinated Biphenyls (PCBs) which were banned in Canada in 1977, and Perfluorinated Compounds (PFCs) found in non-stick coatings, and organochlorine pesticides.
All of earth’s inhabitants have the right to gestate in a healthy environment free from toxic chemicals. Chemicals that are capable of travelling into the placenta have no place in any product, any workplace or any environment.
So I say that cancer prevention does not live in this cathedral of consumerism.
[4] WHO – State of the science of Endocrine Disrupting Chemicals – 2012 http://www.who.int/ceh/publications/endocrine/en/index.html
[5] Pre-Polluted: A Report on Toxic Substances in the Umbilical Cord Blood of Canadian Newborns. Pollution in Minority Newborns Environmental Defence. http://environmentaldefence.ca/blog/canadian-children-are-being-born-pre-polluted
Pollution in Minority Newborns. Environmental Working Group. http://www.ewg.org/research/minority-cord-blood-report. http://www.ewg.org/research/minority-cord-blood-report/bpa-and-other-cord-blood-pollutants
Maria Arnold
Department of Environment, Food and Rural Affairs
Full text is available here (pdf).
Maria told us about Client Earth’s work both on legal side as an environmental law organisation and also on their healthy air campaign.
Client Earth has been trying to engage the public and communities in tackling poor air quality which accounts for over 29,000 deaths each year. That is more than deaths from obesity and alcohol combined – yet poor air quality (PAQ) consistently comes out bottom of the list if you ask most people what has the worst health impact in relation to premature death. Even a group of 100 MPs surveyed recently put PAQ at the bottom of the list. In fact, air quality is second in the list in terms of amount of premature deaths caused.
Maybe one of the reasons it’s so hard to get dialogue around air quality is the fact that the UK has failed to meet all the legal targets for air quality which are established at EU level. It’s much easier when it comes to ill-health to blame the individual for their bad diet, smoking or lack of exercise instead of the polluted air. And PAQ is not just responsible for respiratory problems such as asthma and Chronic Obstructive Pulmonary Disorder (CPOD) but strokes, heart attacks, and cancer. In addition PAQ is associated with low birth weight and there is strong evidence coming from London Boroughs such as Tower Hamlets and Hackney that children growing up near busy roads are entering adulthood with smaller lungs. That is something they can’t ‘regain’ in later life and it is a big predictor of life expectancy.
The main cause of this air pollution is traffic and within that category diesel is by far the biggest problem. Diesel causes far, far higher levels of emissions and is the source of two of the most harmful pollutants, Nitrogen Dioxide (NO2), and particulate matter which is very tiny particulates in the air which can penetrate deep into the lungs. The WHO declared diesel emissions carcinogenic last year, in recognition of the evidence for causation of lung cancer.
There is the issue of government policy actually pushing diesel, so in 2010 for the first time we had more diesel vehicles bought than none-diesel vehicles. And that’s because of incentives through tax breaks. Things clearly are going in the wrong direction here.
A recent WHO report stated that significant health impacts are happening even at the current legal air quality limits. We are not even reaching the legal limits in 40 out of 43 air quality zones across the UK. We are failing to meet the legal limits for NO2. In 16 of the biggest cities across the UK we won’t reach the legal limits until 2020 and in London not until 2025 – 15 years after the original legal deadline.
Client Earth has taken DEFRA to court on its failure to meet these legal limits. It’s been quite a long process having gone through the High Court and then the Court of Appeal, without a good outcome. They referred CE to the European Commission as being the enforcers of the law but this is technically wrong, legally speaking. But in May 2013 the Supreme Court made a formal declaration that government are failing in their responsibilities to protect the public from the health effects of air pollution.
Some of the cases more complex questions have been referred to European Court of Justice which may take another year to answer but the result will impact all of the EU member states and may lead to massive fines from the EU Commission.
CE would like low emission zones in every single large town and city in the UK, which would keep out the dirtiest vehicles and boost greener industry but the government refuse to act. CE are increasing public awareness through their healthy air campaign urging people to speak up about poor air quality, without voices demanding cleaner air, the government will not act.
A recent study by Kings College showed that by walking quieter routes in the centre of London your exposure to polluted air was halved. CE encourages communities to map pollution in their areas and highlight less polluted routes. The problem with air pollution is that it is largely invisible, but just because we can’t see smog in London anymore doesn’t mean there is not a problem.
The upcoming air quality review in the EU gives a lot of opportunities to put pressure on government. There are a lot of resources on the Healthy Air campaign website on how to put pressure on your MP, councillors and public health officials in your local authority to take action.
I declare that DEFRA is an organisation where cancer prevention does not live.
Professor Andrew Watterson
Department of Health
Full text is available here (pdf).
Andrew began by pointing out how appropriate it was for the tour to be linking primary prevention with wider health issues outside the Department of Health. But he reminded us that both DEFRA and the Department of Health don’t legislate and produce policy for Scotland, Northern Ireland or Wales but work with the devolved administrations in all three countries. However there is an ever widening gap in how health is addressed in these countries.
What has underpinned the English Department of Health for a long time on paper was a concern about social inequality. When the Black report (1980) came out a number of years ago, it stated the big issues in public health were in relation to poverty, income and income distribution. This was in opposition to the Thatcher government’s line which was not about the main health drivers (the economic and social drivers) but about individual’s lifestyle and victim blaming.
The later health strategies at least pay lip service to ‘life circumstance’ rather than lifestyle, which meant that your health was going to be influenced by your wages, by class, by gender, by age and by where you live.
Prof Watterson thinks there is a lot of tension in the DoH between what the professionals are meant to do which maybe in opposition to what the politicians want to do. The civil servants effectively carry out the policy. Professionals sometimes adopt ‘wilful ignorance’ because of the pressure they are put under knowing that health is formed by social and economic factors. But because the government don’t want to focus on this aspect and instead prefer to focus on individuals and lifestyle, then that’s the route they will go down. So there is a lot of tension in departments like this as to what they should do and what they do do and what they in fact believe in.
A classic example of this at play is although the English government stress the big role played by smoking, food and alcohol in relation to cancer and other health impacts (although nobody is saying these factors don’t adversely affect our health but other factors may be contributing to a much larger degree to these diseases), you would expect the government to take action against the food, tobacco and alcohol industries. But they say they don’t want to interfere, only utilise voluntary agreements and take a ‘blame the individual’ approach.
But it depends what kind of prevention policies we want and how they are formed, do we want clear guidelines and government enforcement and then decision making under that or do we want to say, well it’s up to the individual. But instead of putting increased pressure on industry government put increased pressure on individuals, who may not have any options.
There are quite a lot of good public health measures coming from the EU, very pertinent to cancer prevention. The EU is taking a similar line to the WHO, that is, talking about upstream medicine (we should talk about upstream health) and downstream medicine and health. And what the WHO and the EU says is that we should all be upstream in other words, you look at what causes diseases and you prevent people falling ill. You don’t wait for them to fall in the river of disease and try and pull them out and treat them for their illness further on downstream. So there is a real tension at the moment between governments who really focus on the downstream side of things rather than the upstream side.
This approach is illustrated quite strongly if we look at breast cancer – if you’re a woman and you follow the government logic on breast cancer, with the right sort of diet, don’t drink a lot of alcohol, don’t smoke, don’t not exercise, and then everything will be fine because that’s where a lot of the key risk factors are.
But ironically quite a lot of researchers are saying the issues maybe genetic, but if we are looking at the big cancer picture research suggests we also need to look not only at genetics but at epigenetics and epigenetics is about environmental influences on people. Researchers are saying the big agenda is what the environment is doing to us in different ways, but now how we define the environment is quiet complicated.
It could be a social environment, a physical environment, or an interaction of all environments. All of these things may come together so if we want to address the big health issues, what we need to do is join up those strategies in ways that can influence most people.
Round the corner a little way from here was an epidemiologist called Jeffrey Rose. He made the observation that if you wanted to affect public health what you needed to do was to look at large populations exposed sometimes to quite low level effects of things, rather than small populations that were exposed to large effects.
So if we are looking at large populations/low level effects in fact we may well find that this is a major cause of disease. And if we are looking at cancer prevention, and if we are thinking about environmental and work environment factors perhaps that’s where the focus should be. There are arguments about strategies and there are arguments about policy.
Andrew told us a little story about pesticides and the DoH. The DoH is meant to co-ordinate the work with regard to public health issues that go on across the board, so DEFRA and HSE may feed in expertise but then the DoH decide what action should be taken.
In the 1980’s there was concern about pesticides and herbicides particularly 2,4-Dichlorophenoxyacetic acid (2,4-D). These pesticides were linked to agent orange used in Vietnam, they had been sprayed so there was a combination of 2,4,5-Trichlorophenoxyacetic acid and 2,4-D. There was a lot of evidence in the 1980’s to indicate that 2,4-D was a possible human carcinogen causing soft tissue sarcoma and non-Hodgkin’s lymphoma among other things.
So a group went along to the DoH and talked to a medic there, and although he said the science was very interesting and they might well have a case, once the DoH admitted there’s a problem with a chemical, this would be like the hole in the wall of dam. Everything else will go, so the DoH will never actually admit that there are problems.
If you run that forward and today we heard about DEFRA and its line on diesel. Diesel has been known as an animal carcinogen for a long time in scientific literature and now the International Agency for Research on Cancer (IARC – funded by the WHO) say it’s a human carcinogen. So why now isn’t the DoH taking a lot of action with regard to diesel problems?
The Organisation for Economic Co-operation and Development (OECD) say that the biggest agenda we’ve got globally is diesel, we are spewing out this carcinogen which also causes major respiratory problems, so it ought to be the top public health issue. But if you look for action from the Doh and related ministries, you can’t see any anything.
We could say the same thing about formaldehyde in furniture and consumer products (another IARC carcinogen), the DoH have no views on this. They will have their expert committees, they will have the scientists – which I would argue in some instances are engaged in wilful ignorance – they don’t stand up and say there is problem. They make recommendations and minsters basically ignore them.
We know diesel is a carcinogen, recently research has shown that shift work has affected males and females, in terms of carcinogenicity. The European Union says we need to take action on things, but the DoH says, none required. We heard about Bisphenol A (BPA) where the French and Canadians are acting, the DoH says, not a problem. What we need to do is not engage in upstream medicine, what we need to do is take action whether every t is crossed and every i is dotted. So you will find that departments like DoH are 10, 15, 20, 30 years behind in decision making on substances and processes that are known to be a particular problem.
We need to look at the standards that we set, and we need to look at the policies that we develop. And although there are lots of good people in this ministry you don’t hear about what they are doing. And that’s why I would also say, we have a look at the UK wide agenda, see what other countries within the UK are doing, because they have social injustice, health inequalities, and environmental pollution somewhat further up the agenda, and are taking action that I don’t think is happening in England.
So what we want are UK actions by the DoH, DEFRA etc. All of these things link up, and we must address life circumstance issues but also address physical environment. I say that cancer prevention does not live at the Department of Health.
Professor Andrew Watterson

Department for Business, Innovation and Skills
Working lives
The Department of Business, Innovation and Skills (BIS) represents the business and working lives section of the toxic tour.
Andrew talked about the complex interactions when we look at cancer. In the old days, the view was you get an external cancer causing substance, its hits the body and that was it. But now we need to look at the bigger picture, now what you get is the issue about multi causality and complex interactions.
This is really important in the context of cancers like breast cancer but also the neglected cancers, such as prostate cancer for men. With breast cancer it’s important when menstruation starts and when it ends, how many children you have, and what your family history might be. These are all things that the breast cancer charities focus on but in fact what might happen is that at different stages, you could get different hits.
Scientists are finding with chemicals like endocrine disruptors, mentioned at the start of the tour, they may in fact affect the woman when she is pregnant, crossing the placenta barrier. They may also affect an infant when they are young, and they may affect a woman as she gets older. We know about external factors, things like HRT etc. They have been relatively well studied, although there are still debates there about what their effects would be. But what about the external insults?
What a group of scientists at Stirling University have been doing, in conjunction with some US and Canadian researchers, is to map through the work history of women who have certain types of breast cancer. Bearing in mind that Dr. Julia Brody (from the Silent Spring Institute) and others have said there are 232 chemicals that they knew of, that could cause breast cancer.
And the work history, in fact, actually goes beyond the workplace. Because in Canada the mothers exposed to potential breast carcinogens, may have used these chemicals and could have exposed the child in the womb. Then if the children live in farming areas, they could be exposed via pesticide spraying. Then there could be critical windows of exposure, for example during adolescence, and during the teenager years they continue to get insults from harmful chemicals. When they go to work, or maybe they work on a farm, they would continue to get the exposed to agro-chemicals.
What we found in Canada was that the women often lived on farm, worked in the agricultural industry, and then went to work in the metal industry, in the health service, or in the car industry which is why we are quiet interested in studying places like Windsor, Canada. In the car industry, we discovered they were using a whole set of plastics and polymers such as vinyl chloride and a range of other chemicals that in laboratory tests are known to cause breast cancer.
This was a large study group of over 1,000 women in the case group, against the control group of 1,000 women. Detailed work histories were taken and we found there was a 4 fold excess of breast cancers in many woman in the food packing industry. The only thing that we could pick out that seemed to be significant there was that they soften their plastics with Bisphenol A (BPA). Evidence has been growing and giving a consistent trend showing that BPA will affect human cells and in laboratory tests is a human carcinogen.
Occupation is grossly neglected in terms of looking at all cancers, but if you were looking at breast cancer and exposure, you wouldn’t stick a monitor on a woman to see if the levels of exposure to various chemicals at work were over the limit or not. Recent studies into some of the chemicals used in the plastics industry have shown that the pre-determined safe exposure levels can be met but these exposures are lower than the official levels, yet the women have higher levels of these chemicals that you would expect in their blood. So having exposure standards won’t work, so what do you do? You focus on the woman and ask whether we should unpack all of these things like genetic susceptibility or do we focus on the carcinogen.
The smart thing to do is to go for the carcinogen rather than the cancer. Because there are many different sorts of breast cancer- some are oestrogen positive, some oestrogen negative, some are progesterone positive so the biochemistry is extremely complicated so it definitely makes more sense to focus on the carcinogen.
If we consider what focus there is on occupational cancer generally and on breast cancer in particular. What you will find in the UK is that there is a miss match between what’s going on internationally, what’s going on in Europe and what’s going on here.
Internationally the World Health Organisation (WHO) and Europe are flagging up environmental and occupational causes of cancer as a big issue and we can’t actually separate them, because what happens in the work environment is going to seep into the wider environment.
But when you look at the chemical testing processes, even though Helen has quite rightly flagged that for consumers there is a lack of rigour, when you look at the workplace, there’s even less rigour. So there’s more testing done to protect the consumer even though we know still a lot of toxic products have got through, but if we consider the workplace, we find that even less testing goes on.
The estimate from the WHO is that something like 7-17% of all cancers in the world are environmental caused. So if you consider who’s going to be exposed longest to the highest levels of a substance, it’s going to be people in the workplace. So it’s worth bearing that in mind. We must have this caveat at the back of our minds as well, that we are talking about multiple insults.
Wendy Chavkin is an occupational physician from the US who coined the phrase double jeopardy and double jeopardy is where a woman goes to work and is exposed to a whole range of hazardous substance including carcinogens and then she comes home, cleans the house and does a whole range of domestic tasks and then gets exposed to another set of carcinogens.
I think probably we should talk about quadruple jeopardy, because we are talking about what people do in the home, what they do at work, what’s in the wider environment and then what might be in our food and drink, so there could be a whole set of routes of entry, for a whole range of carcinogens.
But in the context of the workplace, the assessment has been historically that most occupational cancer pales into insignificance against these lifestyle cancers – or what I would call life circumstances. It all goes back to Doll and Peto who estimated that 4 – 4.5% of all cancers were down to work and since the 1980’s there has hardly been any revision of that figure. Now in the US and Europe people are really seriously questioning that figure.
In the UK the HSE deals with occupational work across the UK, that includes Scotland. They have done some re-estimates and are coming up with a figure of 5-6% of cancers that maybe work related. And within that figure you will find a number of breast cancer cases. But even when Doll and Peto produced the lowest figure of 4.5%, 4.5% of the population at work getting cancer is a big issue. So we are not even taking action on the biggest factor for cancer in the UK, work.
The European Agency for Safety and Health, (EASH) a mainstream European body, are saying that 18% of all cancers are down to occupation. They have a much smaller figure for women, but that’s because they don’t show up in the statistics, the standard response is we focus on the man’s occupation, not the women’s. It’s only been in the last few decades that information has been coming out about women’s occupational cancer.
The UK estimated recently that there several hundred deaths from breast cancer due to work, this was in their officially commissioned research. So you would think that that would then trigger a big campaign, women dying from occupational breast cancer. But the British government is not too sure.
The Danes have shown that shift work and breast cancer are linked and they compensated women. But that’s in Denmark, here we need to do our own research because we must assume they think that British woman are different to Danish women in some respect and they have actually kicked it into the long grass.
So nothing is being done, this is against a backdrop in terms of the pink ribbon campaigns – we have seen a 70% increase in the number of women with breast cancer between 1970 and now. In the last full decade between 2000 – 2010 there’s been a 6% increase, we’ve seen breast cancer incidence rising all the time, so from 1 in 8 veering down to 1 in 7 women will contract that disease.
We are talking about very significant percentages of women contracting breast cancer. Bodies like Cancer Research UK are saying that 40% of breast cancer is down to our diets, it’s down to alcohol, it’s down to food, but effectively they have been saying that for a long time. That the majority of breast cancer is not explained but whatever is causing it, it’s not work and it’s not the environment.
So you juxtaposition that, with the growing list of chemicals and activities like shift work physical exposure and management systems that are known to cause cancer definitely or probably in humans, that list is growing.
A lot of work has been done by environmental groups and what we know about endocrine disruptors from highly respected researchers from good places like Tufts and Ivy League universities in the US, is that minute quantities of these chemicals may have an effect. And if we look at where you are getting your exposure to endocrine disruptors from, males as well as females (because EDCs affect the prostrate as well) you get them in the workplace, and you are going to get them in consumer products. In fact there’s a whole set of other exposures that may play a role.
So that’s why bodies like the Alliance for Cancer Prevention and others are saying we need a new strategy to address this. There’s been an under prioritisation.
There is this strange term – which is about secondary prevention – which is effectively screening, that’s not prevention. I am not in any way addressing the importance of screening where appropriate and effective but we have seen a big debate about this and the evidence from the scientific community seems to be shifting quiet significantly towards the hazards of screening and away from the benefits. But you would think the Dept. of Health and others would have a strategy to address this?
As we are outside the BIS it’s important to say that it doesn’t regulate Scotland and Wales, but it is incredibly important as the ideological driver of deregulation, what’s euphemistically called better regulation . And what BIS wants to see is economic growth prioritised in public health bodies, in the Health and Safety Executive, in DEFRA, etc what it doesn’t want to see is precautionary , prevention and inspection brought in.
In Denmark when the results on elevated rates of breast cancer linked to shift work came out, they sent their labour inspectors (equivalent to our health and safety workplace inspectors) to work. They started enforcing the European regulations to ensure there weren’t abuses on shiftwork and that there was proper health surveillance.
What we see with BIS is that they are reducing the emphasis given to even basic occupational health and safety activity. There is a lack of action on occupation carcinogens, inactivity on diesels and on endocrine disruptors, and a rejection of the precautionary principle. They will continue to be like that until we count the bodies.
If we are looking at workplaces, we often find, that industries that produce these carcinogens, have gone in 10- 20 years and what’s left are the people that are adversely affected. There must be better ways of addressing this and ministries like this are critical.
I say that cancer prevention does not live at BIS.
Hilda Palmer
UK Parliament
Full text is available here (pdf).
Hilda began by reminding us that at least 20% – if not more – cancers are caused by occupational and the environmental exposures and even if we take a very moderate 12% of cancer as being caused by work, that’s 18,000 deaths a year. And as we heard about the deaths from air pollution that’s not a number we would hear often, and it’s caused by chemicals that people are exposed to at work, and practices like shift work amongst other things.
Hilda spoke about what trade unions should be doing to tackle occupational cancer and the workplace, but before that, she reminded us, that currently we are in a situation where the government is attacking the whole health and safety regulatory and enforcement requirement. So the laws that workers fought for, for hundreds of years and the enforcement systems that we built up to make sure the employer obey those laws, these are all being broken down and the people that are inspecting the employers to make sure they are being compliant to the basic laws, are all being cut tremendously.
What is happened as part of this is that occupational health, all the things we are talking about in terms of cancer that is absolutely being wiped off the agenda.
So when we are talking about what can Trade Unions do, we have to understand that it’s in this environment, so not only are trade unions fighting for their member’s jobs, pensions and wages etc, but they are also trying to fight for their health and safety. And they are fighting in a situation where the government is removing the regulations and enforcement on the employers to make them provide safe and healthy workplaces. The government is not at all interested in doing anything about occupational cancer.
Hilda and Helen recently attended the Health and Safety Executive (HSE) conference on cancer, and occupational disease. They protested outside because of the HSE’s dithering, denial and delay on all sorts of occupational issues but particularly those relating to women.
It was the most complacent conference you could possible imagine, in terms of the work they are doing on occupational health and specific things like shift work. Because what they are doing is absolutely nothing. That’s the situation in which workers and trade unions find themselves in.
That’s not to say that trade unions shouldn’t be doing a great deal more, some trade unions are doing quite a lot of work on cancer such as Unite, and the GMB who are doing work on vehicle exhaust emissions affecting drivers and delivery workers. Others like UCATT are working on asbestos and silica dust. Unison and the Royal College of Nursing are beginning to do some work on shift work and breast cancer. The teaching union, NASUWT are doing quite a lot of work with other unions on asbestos in schools. Because an unfeasible large number of people work in schools, and it is not an environment you think they would be exposed to carcinogens like asbestos.
In general work on chemical hazards has gone off the boil and no one is really setting the agenda, or speaking out very clearly about it. And that is what Trade Unions could be doing much more of, raising the issues, raising the profile, raising awareness among their members in the workplace and talking about these issues a great deal more.
As Andrew Watterson and other people have said, when the WHO said that diesel exhaust emissions are a definite human carcinogenic, the Trade Unions didn’t make enough of this and what that could mean for their members. And if the TU’s are not coming out strong on this, then they are not pushing anyone else to do so.
At the moment the government hasn’t removed a very good piece of legislation we have called the Control of Substances Hazardous to Health (COSHH). In fact they have been very poor on enforcing this piece of regulation which says that all employers have to assess the risks of all chemicals in their workplace for any risks they pose to workers health, and if they pose a risk such as being a carcinogen, endocrine disruptor, etc they immediately have to look at eliminating that risk if they can and if they can’t, they have to look at substituting it with something safer. If they can’t do that then they have to look at engineering controls to reduce the exposure to all the people in the workplace – a collective intervention. And only as a last resort can they put people in personal protective equipment. These regulations have been there since 1988, but they are incredible badly enforced and yet if they were enforced then an enormous amount could have been done, in terms of substituting carcinogens and other hazardous substances in the workplace over the last 20 odd years.
It’s not only the enforcement authorities that have failed there, but also the Trade Unions to really fully use this piece of legislation. There is a lot of information on occupational cancers, a large percentage produced by Rory O’Neill through Hazards Magazine, on what’s safe to use, which chemicals cause what type of cancers and what processes they are used in. But a lot of this information isn’t getting out to the TU members and workers in their workplaces.
There are carcinogens in all workplaces but there isn’t really enough support on getting employers to carry out the risk assessments or identifying the carcinogens and then doing something about them and this is also true of issues like shift work.
In other countries there are progressive initiatives such as Toxic Use Reduction programs where trade unions can get much more behind the idea that we are trying to get all hazardous chemicals out of workplaces or if not we should be looking at how we reduce these. In some states in US there are laws that help them to do that.
We could be arguing for sun-setting (phasing out) of carcinogens and other hazardous chemicals, we could be putting pressure on chemists and people to design safer chemicals and provide more information about alternatives.
There are very good websites in the EU already doing that, one called Subs-port where you can look up chemicals you are using and find safer alternatives. And we should also be looking at zero usage of toxic chemicals, using as few toxic chemicals as we can, which also links with the green agenda.
We haven’t as Trade Unions argued enough for this and we haven’t pushed the employers hard enough. We need a regulatory and enforcement framework that is very strict and actually works which then drives innovation, drives change, and drives the manufacturers to come up with safer chemicals and safer processes. There are all sorts of ways in which this could be done.
And some of these are very simple. For example, in laboratories in Denmark they used to use acetone in the final glassware wash so they would dry quickly. Acetone being toxic, the lab assistants came up with a solution, why don’t we buy three times as much glassware and then things could dry as slowly as they like. A very simple and quite an elegant solution.
Where workers are involved in finding the solutions and once the framework is set up, where we actually say it’s not good for workers to be exposed to toxic chemicals, or any chemical in excess, (and it’s certainly not good for them to be exposed to carcinogens) only then do we encourage workers to support that.
But this doesn’t exist, and isn’t being imposed by government, Andrew and other people have told us how our ministries and how our government are letting us down, that is a big problem.
But there is an opportunity for trade unions and the Hazards Campaign to make more links between workers and communities in relation to toxic chemicals. If chemicals are being used in manufacturing process ie plasticisers like Bisphenol A and then they escape into the community and potentially getting into peoples food and water, then we should be involved in making a common cause with community groups.
We have to push COSHH hierarchy, elimination, substitution, engineering controls, toxic use reduction, the zero use of toxic chemicals, and we have to push the precautionary principle. We have to talk much more about inequality – health inequalities, and social inequalities – given that some workers are exposed multiply to toxic chemicals in their workplaces, and in their environment.
So although there is a lot of really good work going on, there is much more we could be doing. We are in a really vile environment at the moment where this government doesn’t care about our health, we could all die at work and they wouldn’t really care about us.
They are setting a framework for health and safety at work which will mean in fact that more people are going to be exposed to more toxic chemicals and more harmful substances and unhealthy work practices such as shift work.
Hilda ended by introducing us to the work of one of our colleagues Simon Pickvance who worked in Sheffield where he set up a pioneering way of looking at workers health. He worked in doctor’s surgeries talking to people when they came in with their health problems, taking work histories from them and then discussing these histories with the doctors so the doctors had more of an idea why people were getting ill and what was causing it. Then they tried to work with Trade Unions and people locally to discuss how to tackle those issues. They did really brilliant work and through that work Simon identified all sorts of low level exposures to chemicals and mixtures of chemicals that caused bladder cancer and a whole range of cancers. But the HSE will not accept this exists.
Simon knew far more about cancer and he has given us tools to reveal this that are much more sensitive than the rather crude epidemiological studies that actually look at small groups of people, in workplaces where they have worked for 30 yrs, rather than huge numbers of people doing a whole range of work, where they are receive smaller exposures.
Simon actually died last year of mesothelioma caused by asbestos because he worked on a building site to raise money while he was doing this pioneering research. Thank you.
I say that cancer prevention does not live at the House of Commons.
Deborah Burton
UK Parliament
Deb began by questioning why campaigns matter and why we have to work so hard to punch through to our elected leaders on this issue. Having heard from Andrew and Helen about the scale and level of exposures to toxic chemicals all around us – lifelong low level exposures to hormone disrupting chemicals’ – and also from Andrew about the ‘wilful ignorance of government departments to act on the evidence’, it is fitting that we come to a close here on the walk, at Parliament as they are the final decision-makers on this. But what hurdles are in the way?
Deb first came into this issue in 1997 through a Channel 4 documentary called The Lindane Legacy, by Hilary and Ray Dawkins. And was shocked to discover this ‘new’ link between the environment, pesticide exposure and breast cancer. She called the film-makers to ask if she could get permission to organise a screening of the film in parliament for ‘Blair’s Babes’ – the new female intake of 1997. They agreed and it was then she discovered that there was already a Ban Lindane campaign and UNISON was central to that campaign along with WEN, Friends of the Earth, the Pesticides Action Network, the Soil Association and others.
In 2002 we won the Lindane battle when the EU banned it. But one comment stuck in Deb’s head at the time of the House of Commons Screening. It was from her MP’s PA (her MP being Ann Keen, a former nurse and in the Health Department). The PA had expressed surprise as the Lindane issue was being discussed. She said that she was amazed that there was this link, to paraphrase her, all she saw was a trail of drugs reps coming through the door, but she had no idea there was this other dimension to the issue.
There has been a lot of news recently about revolving doors where the link between industry and government is shown to be very close especially in terms of shaping legislation ie former accountants being seconded to advise government on tax affairs. On this issue of breast cancer, it is fair to say that if you are NOT about treatment or drugs, or PINK and fundraising, it’s very hard to get a place at the table to make the case for prevention or for research into prevention or attention paid to the environmental and occupational links to cancer, including breast cancer.
Now, a recent report from the WHO and UNEP considers EDCS to be: “a very serious and immediate threat to human health and wildlife and signals the urgent need for effective regulation and testing of these chemicals”. The report estimates that as much as 24% of human diseases and disorders are due at least in part to environmental factors which include chemical exposures. “Many endocrine diseases and disorders are on the rise and the speed at which they are increasing rules out genetic factors as the sole plausible explanation”.
As the Alliance for Cancer Prevention says, some 800 chemicals are known or suspected of interfering with our hormones. Yet only a small fraction of these chemicals have been tested and our daily exposure to them is widespread.
So let’s just ask the question: how do we get this in front of elected reps? How do we access the political system so that this information is taken as seriously as the other dominant aspects of the debate?
A way to understand these relationships between our elected reps and the vested interests is to look at the All Party Parliamentary Group system. This is where MPs join groups that are of interest to them and which are the ground level of debate and discussion. The APPGs are often administered by external groups which have a knowledge of the issue . All the info below is taken from the House Commons website.
1. The APPG on Breast cancer: is administered by Breakthrough Breast Cancer. Breakthrough receives sponsorship from AVON (and we heard about the complicated story of cosmetics and breast cancer in Helen’s talk also the film Pink Ribbons Inc. which explores ‘pinkwashing’) and they also get funding from drugs companies including Novartis and Roche. Roche donated £2,500 for the Breast Cancer APPG Annual Dinner, £10,000 to support our work through Campaign Advocacy Networks, and £7,500 for our Annual Reception. Roche also sponsored the Westminster Fly-In (oganised by Breakthroughs CAN group) for £15,000. (Total £35,000).
The APPG on breast cancer has as its Vice Chair, Baroness Delyth Morgan a long time breast cancer campaigner. Delyth Morgan oversaw the growth of Breakthrough Breast Cancer to become a major figure on the breast cancer scene. She is also Chief Exec of research charity Breast Cancer Campaign which has a page on its website looking at risks established, possible and doubtful.
DOUBTFUL RISKS to breast cancer page says
Factors that are not thought to affect your breast cancer risk:
Pesticides or other pollutants
- There is no convincing or consistent scientific evidence linking exposure to pesticides or other pollutants to an increased risked of developing breast cancer
- Many studies have looked at different pesticides or pollutants and their effect on breast cancer risk but as we are exposed to low levels of many different pesticides or pollutants over a lifetime, it is difficult to know which, if any, of these influence risk.
I think it is shameful that these organisations can be so ‘wilfully’ ignorant of the evidence out there. Shame on them.
2. The APPG on Cancer – Macmillan Cancer Support provides the secretariat to this group. Delyth Morgan a member of this APPG also. Macmillan lists benefits received as:
| BENEFITS RECEIVED BY GROUP FROM SOURCES OUTSIDE PARLIAMENT |
| Macmillan Cancer Support (a charity) provides the secretariat to the group (co-ordinating the work of the group, providing the website for the group, and organising the annual Britain Against Cancer conference). Donations received towards the Britain Against Cancer conference held on 11 December 2012: £2600 from Sanofi-Pasteur, £4600 from GlaxoSmithKline (registered October 2012); £4600 from Roche (registered November 2012); £4600 from Janssen, £4600 from Novartis, £6700 from Pfizer (registered February 2013). |
3. The APPG on Chemicals
This APPG is administered by The Chemical Industries Association (CIA) which is the largest organisation that represents chemical and pharmaceutical businesses throughout the UK. They represent all sizes of chemical and pharmaceutical businesses and approximately 70% of their members are overseas headquartered.
On the Friday before our walk they were tweeting about pushing Shale Gas for UK.
4. The APPG on Health
The secretariat support for this APPG is Policy Connect they are supported by a wide range of chemical and pharmaceutical companies.
| Group’s website. |
| BENEFITS RECEIVED BY GROUP FROM SOURCES OUTSIDE PARLIAMENT |
| Policy Connect (a not-for-profit organisation) acts as the group’s secretariat. £8400 membership fee received from each of the following: AstraZeneca, Bristol-Myers Squibb, Xograph (registered September 2012); Milliman, Novo Nordisk, Takeda, Abbvie, Ascribe, GSK, Napp, Northgate IS, Nutricia, Healthcare at Home, Novartis (registered March 2013); Sanofi-Pasteur MSD, Lundbeck Map of Medicine, Pfizer, Merck Sharpe and Dohme (registered June 2013). |
To go back to 1998 now we know why, at the time of the Lindane Legacy Deb’s MPs PA said she knew nothing of environmental links to breast cancer. Is it any wonder that the UK Government is so weak on taking note of the ‘precautionary principle’ when it comes to this issue of environmental links to cancer, to breast cancer? Or that a drug, Tamoxifen is now being offered to 500,000 women that are perceived at risk (despite its side effects) a drug given to reduce oestrogen while they wilfully ignoring EDC’s (chemicals which have the ability to interfere with how oestrogen is broken down or accumulates in the body) which Deb thinks might be one of the primary causes.
Add to this media ignorance, the saturation of pink, fundraising for treatment and research that does not include primary prevention, and is it any wonder that our side of the argument is closed down by the predominant discourse of drugs companies, mainstream cancer charities, business and by extension, government?
In 2007/8 I was working on the tax campaign and we could not give it away! Now? It is everywhere, tax is ok, even sexy! Very big and powerful players are being challenged, tax haven, banks, business and wealthy individuals.
One day we will see the same happen for this issue. ..
And maybe the EU will be the mechanism to force the UK government’s hand on this.. Deregulation got us into the banking mess. Regulation is key.
Dr. Ana Porroche-Escudero
Emmeline Pankhurst statue
Ana began by presenting 3 reasons why the pink discourse is toxic. But beforehand she reminded us that the goal of breast cancer awareness campaigns is to empower women so they can make informed choices. Empowerment demands realistic, evidence-based clear information about the real potential harms and benefits of the different therapeutic options.
At present, she argues that the way in which the pink discourse is rephrased undermines the empowerment intent through fear mongering, misinformation, and trivialisation of the disease.
First cause of toxicity: Pink discourse uses fear-mongering tactics that plays on women’s fears; fear of our potential carcinogenic breast, fear of our children losing their mothers. Also, fear of being unsexy or dying.
Misinformation is key here. Statistics and personal narratives (often from celebrities) are distorted, misused, or left without context, sometimes to simplify information, sometimes to attract headlines. A fascinating article to read in connection with this is by Woloshin and Schwartz called “How a charity oversells mammography”. The result is that we have the impression that all of us are at super high risk of developing breast cancer. But, the fact is thatbreast cancer is not the leading cause of death for women but is a leading cause of fear because it has been oversold.
For example, some of the controversial messages that we receive imply that:
- We have a massive risk of having the faulty genes. This is false, only 1% of the population might have them and only 5-10% of cancers are genetic.
- Mammograms prevent cancer. False. They help to detect cancer earlier but don’t prevent women from getting a tumour. In addition, screening detects about only 1/3 of all breast cancers and about 1/3 of diagnosed breast cancer is not cancer. It is over-diagnosed and over-treated to the extent that H Gilbert Welch in his book ‘Should I Be Tested for Cancer?’ argues that some women may become sick as a consequence of treatments and not cancer. More often than not women are still not informed of the risks before screening, nor of the poor quality of evidence of the chance of benefitting from screening.
Another toxic characteristic of the pink discourse is that it trivialises the disease on many levels. For example, the women portrayed in breast cancer campaigns and ads tend to be beautiful, young, happy and healthy. Two things here: one, the risk of breast cancer increases with age and average age at diagnosis is 61. Only 5% of cases occur in women under age 40. Two, cancer is not sexy. As Barbara Ehrenreich puts it in the film Pink Ribbons, Inc : ‘breast cancer is horrible’ and it has a tremendous impact on women’s health on a physical, emotional and spiritual level and yet ill-looking women are encouraged to use wigs, makeup or prosthetics to ‘regain’ femininity. The many women who don’t want to comply with this stereotype are labelled as depressed, butch, anti-erotic, or in denial.
These representations of the cheerful woman limit our ability to comprehend what it’s really like to face the disease, live with medical uncertainty, and accept the difficult realities of risk, pain, recurrence, treatment, disability and even death.
Pinkwashing is the second toxic byproduct. According to the organisation Breast Cancer Action, pinkwashing is “when a company or organisation that claims to care about breast cancer, produces or sells products whose ingredients are linked to the disease”. Two clear examples are Esteé Lauder Cosmetics and AstraZeneca Pharmaceuticals. Both companies are hardcore promoters of the cause. Yet many of Esteé Lauder’s cosmetics contain carcinogenic chemicals. In a mind-blowing article ‘Cancer Butch’ by Lochlann Jain (2007) citing Barbara Brenner, who reveals that AstraZeneca which manufactures the controversial breast cancer drug Tamoxifen, also produced pesticides linked to breast cancer, including “acetochlor, a known carcinogen and a $300 million market”.
And where does our money go? The Breast Cancer Consortium and Breast Cancer Action highlight that many companies who sell pink products to donate a percentage of each sale to breast cancer programs don’t state which organisations will benefit from the money. Moreover, we don’t know how these organisations spend the money and if it goes to addressing the structural causes of the epidemic. Breast Cancer Action writes on its website “At other times companies that donate money to support breast cancer programs put an arbitrary ‘cap’ on their maximum donation. Once the maximum amount has been met, the company may continue to sell the product without alerting customers that no additional funds will be donated. This means you may be buying a product for which none of your money will go to a breast cancer cause but to the company”.
Perhaps one of the most infamous examples given by the late breast cancer activist Barbara Brenner was the American Express campaign in 2002. After American Express agreed to donate a penny each time an American express card was used between September and December, Breast Cancer Action denounced that even if a card member spent $1000 on one purchase, American Express would still only donate a penny for that one use, dismissing such a donation as less than worthless.
Rather than promoting fear about women’s bodies and life style factors, we should think about what is really contributing to the widespread toxicity of breast cancer and demand better information and more research. To conclude her talk Ana suggested that Breast Cancer is more than an epidemic of disease. It is an epidemic of vested interests.
Breast Cancer prevention lives here at the Emmeline Pankhurst statue.











